Our Work
Church of Saint George, Lalibela, Ethiopia
ETHIOPIA
As the second largest country in Africa with a population of nearly 110 million, Ethiopia bears an enormous burden from tuberculosis and lung disease. A 2009 report from the World Bank titled “Ethiopia: Improving Health Service Delivery” notes that in efforts to improve healthcare delivery and outcomes, “the key constraint was the lack of specialized doctors” to provide basic services at the primary and secondary care level.
Of the 22 high burden tuberculosis countries, Ethiopia is 3rd on the list in Africa, and 8th in the world with an annual incidence of 261 cases/100,000 population. These cases include the emergence of multidrug resistant pathogens (MDR-TB) and extensive-drug resistant (XDR-TB) pathogens. Besides tuberculosis and other lung infections, rates of non-communicable lung diseases such as COPD, asthma, and lung cancer are also rising and contributing to mortality and morbidity. The average life expectancy in Ethiopia is 65.48 years.
Health care remains critically underfunded in a country that ranks among the lowest in per capita gross domestic product. Most of the health care is delivered by generalists at health posts, health centers, and general hospitals. The ratio of total physicians to population is less than 1:10,000 persons (2:10,000 in Kenya, 4 in Uganda, 8 in South Africa, 19 in China, 25 in the United States and 40 in Switzerland).
In Ethiopia, specialists are rare (1:63,000 population). Even still, this number is inflated because general internal medicine physicians are counted as specialists. Additionally, the economic and structural medicine challenges such as the lack of transportation infrastructure, the lack of rural hospitals, and the lack of trained pulmonary physicians also contributes to the prevalence of treatable and preventable pulmonary diseases. Prior to 2013, there was only one pulmonologist in Ethiopia.

MISSION
EATI'S GOALS
- To address the dire need for pulmonary and critical care specialists in the country
- To ensure the fellowship training program is self-sustainable by EATI-trained physicians by the year 2020
- To provide expertise and consultation to the Ethiopian Ministry of Health
In January 2013, the East African Training Initiative (EATI), a two-year fellowship training program in pulmonary and critical care medicine, was launched under the leadership of Dr. Neil Schluger, chief of the Division of Pulmonary, Allergy, and Critical Care Medicine at Columbia University, and Dr. Charles Sherman of Brown University. It is the first training program of its kind in Ethiopia.
The path to this historic moment took two years of careful planning. In March 2011, Dr. Asqual Getaneh the then chief executive of Addis Ababa University (AAU) School of Medicine identified the need to train specialists in pulmonary medicine. However, both local funding and expertise were limited. After discussion with the leadership of World Lung Foundation (WLF)*, a site visit and need assessment by Dr. Neil Schluger and Dr. E. Jane Carter took place in January 2012. Subsequently, with close coordination among AAU, Tikur Anbessa (Black Lion) Specialized Hospital and the Ethiopian Ministry of Health, a memorandum of understanding between WLF and AAU was signed in April 2012. The initial funding for EATI was provided by the World Lung Foundation and the Swiss Lung Foundation.
*World Lung Foundation is a non-governmental organization dedicated to improving lung health in low- and middle-income nations.

PROGRAM
The first year is devoted to clinical care and procedural skills such as spirometry, bronchoscopy, thoracentesis, pleural biopsy, intubation, and central line and chest tube placement. The clinical knowledge foundation is provided by an extensive, year-long lecture series, a wide range of conferences, and daily inpatient rounds in the medical intensive unit and pulmonary wards. Every month, expert visiting faculty members from Europe or North America provide lectures, procedural training, and most importantly, bedside teaching and patient-centered care during rounds.

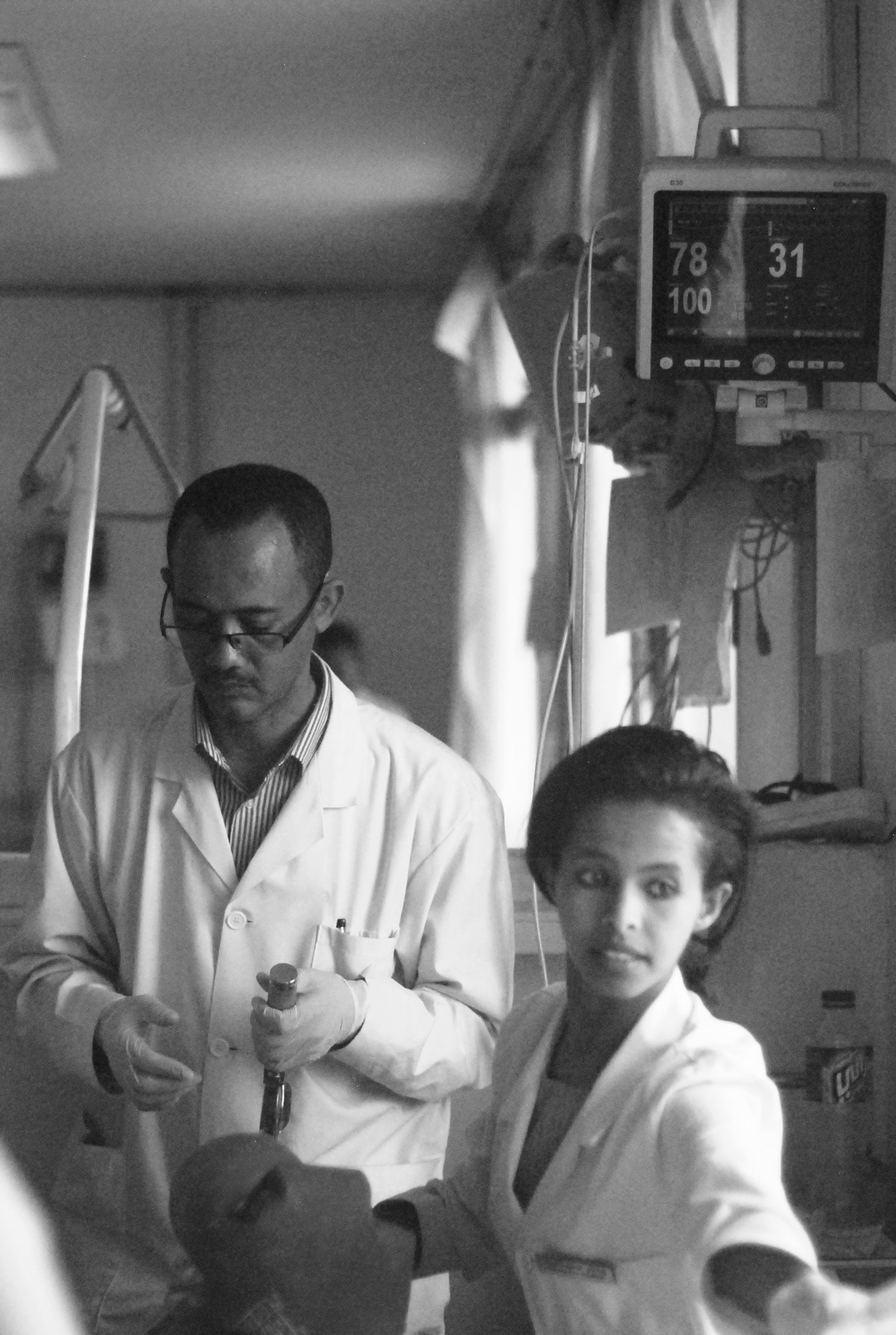
The second year continues the same intense clinical training of the first year with more depth, refinement, and autonomy. During year two, training in research methods and mentored research projects are added. All fellows participate in the Methods in Epidemiology, Clinical, and Operational Research (MECOR) program sponsored by the American Thoracic Society (ATS).
At the end of the second year, the trainees travel to Columbia University and Brown University for a four week observership to learn new medical technologies and a different healthcare system. Before graduation, each fellow must pass rigorous written and oral examinations and achieve high marks on faculty evaluations of knowledge and skill sets.